A team of scientists from the Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore, and Nanyang Technological University, Singapore (NTU Singapore) has developed a quick test kit that can tell if a person has immunity against COVID-19 and its variants, based on the antibodies detected in a blood sample.
For those who wonder if they’ve had an asymptomatic case of COVID or didn’t previously test when ill you might be able to find out soon.
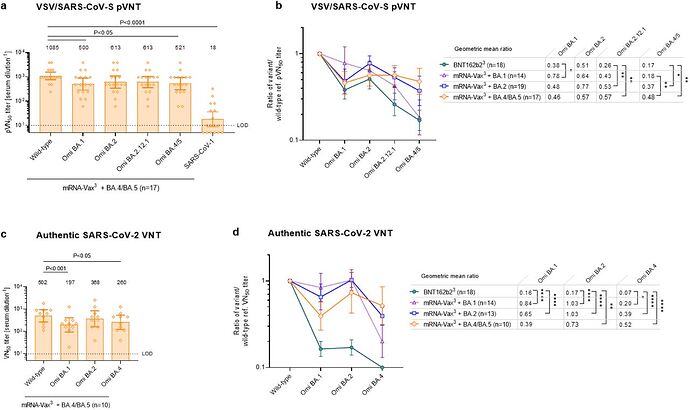
Study compares antibody response in those with vaccination (against the ancestral virus) and vaccination + various types of Omicron infection.
No surprise that vaccination only (with the vaccine for the ancestral virus) gave the weakest antibody response against Omicron variants, while vaccination + infection gave the strongest antibody response against the same Omicron variant. BA.1 (the dominant variants last winter) infection did not give much of a “booster” against BA.4/5 (BA.5 variants are the dominant ones now). Perhaps that is not surprising, since a variant that can break through prior BA.1 immunity that is now common will spread more easily than one that is blocked by prior BA.1 immunity.
A (local to me) consortium is looking into what causes long Covid.
“In comparison to the 2009 flu pandemic, COVID has led to more severe and long-term cardiovascular disease but what was causing that at a molecular level wasn’t known,” Dr. Kulasinghe said.
"During our study, we couldn’t detect viral particles in the cardiac tissues of COVID-19 patients, but what we found was tissue changes associated with DNA damage and repair.
“DNA damage and repair mechanisms foster genomic instability and are related to chronic diseases such as diabetes, cancer, atherosclerosis and neurodegenerative disorders, so understanding why this is happening in COVID-19 patients is important.”
A personal anecdote at school is most teachers have had Covid (no surprise there) and many have new, ongoing, medical problems. It was a bit scary hearing them list off what’s been going on.
Thanks for posting this, it is super interesting and a little scary.
I’m no expert on these types of studies, but wanted to point out some shortcomings the authors identified: small cohort (7 in the COVID cohort), limited age distribution (average age 69), unequal gender distribution (only one female). I hope others in the field are able to research more in this area, it will be interesting to see if the results are corroborated.
I agree it’s a small study but I hope they do more research on the issue now that it’s been identified.
The study was also limited because it used samples from deceased COVID-19 patients who had severe enough disease to be put on mechanical ventilation, but died anyway. I.e. the worst case outcome. Getting samples of heart tissue from living people would be too invasive.
However, even though the study looked at the worst case, the frequency of heart issues being noted as long COVID suggest that heart damage can occur in COVID-19 cases other than those which end in the worst case outcome.
I know Stanford CFS clinic is studying long Covid as well, since there seems to be considerable overlap.
Women are more likely to get long covid in general.
i have not seen these kinds of conditions (diabetes, cancer, etc from the list in the article) described as “long COVID” (actually I haven’t heard of any COVID and cancer relationship in general), and I have seen the physical mechanism for “long COVID” described as being more related to the lungs than the heart.
It’s too bad there’s not a noninvasive way to collect a bit of heart tissue. That seems like it could be such a huge research tool. There is so much more to learn here. Are the results similar for non-severe COVID cases? Are lung tissue samples showing the same changes? Does it vary by demographics? Are there any similarities (I hope not!) with the tissues from the small number of younger males experiencing myocarditis issues post-mRNA vaccine? How about with CFS patients’ tissues?
I worry about Long Covid’s neurological/brain effects.
So does my H who is a neurologist.
The gender ratio mismatch is probably at least partially due to using samples from deceased patients, since men are more likely than women to die from COVID-19 (although probably not 6 times more likely).
YLE writes about Paxlovid studies and results:
Some highlights:
- Effective in older (65+) people but generally not in younger people.
- Rebound is more common with than without, but generally mild.
- Note on drug interactions, since older people are more likely to be taking more drugs for other medical conditions.
- Does not prevent transmission.
- Effect, if any, on long COVID risk is not known.
Is anyone still testing for variants? It seems like there should be a new one by now. Is Omicron still the most prevalent?
Yes lots of monitoring of genomic variants. Here’s the most recent data from CDC
And UK,which has elevated several variants to be ‘variants of concern’ today:
YLE has a recent page where she writes about variants (mainly new Omicron variants):
You can also look at the variant mix over time here:
https://covid19dashboard.regeneron.com/?tab=Variant_Graphs&subTab=Top_Variants_Over_Time_(Select_Location)&Continent=North%20America&Country=United%20States&State=any
Two cousins caught COVID in Thailand and got very sick when they got home in the US. They flew of course, but not yet know they had caught it. I wonder what strain they caught, and how contagious they were in the plane and airport and bus home (masked), especially with an unknown strain.