When you say – no symptoms similar to his first COVID experience - do you mean each time he has had COVID, the symptoms have been less severe?
I mean he had slight symptoms the second time, but virtually none the first or third. By none I mean he is still running six to eight miles a day, or biking or playing pickleball. He has no fever, no aches or pains.
If he has no symptoms, then why did he test himself? He must have suspected something.
Lucky guy. DH and I just had Covid after avoiding it for two years. DH was taking Paxlovid. I don’t know why he was prescribed it since he is 60 without any health conditions. He had fever for two days and was all good after that. I didn’t take any medication and had lower fever for two days, congestion and still coughing. We both had PPP. Honestly I expected it to be less annoying then it was after all vaccinations
One of studies of the US veterans’ health records hinted that a mix of vaccines including both J&J and an mRNA vaccine may be more effective than other sequences of vaccines.
Getting COVID-19 three times sort of goes against that, however. But getting only asymptomatic or minimally symptomatic cases is consistent with it. But how many and which vaccines did he have when he got COVID-19 the first two times, and how did he find out if asymptomatic (i.e. what prompted him to test?)?
I had minimally symptomatic COVID-19 after JJm vaccines (last one 4 months prior). But it took until day 13 for tests to be negative.
He was prompted to test the first time because he was planning on spending a weekend with a friend. (Back when people did things like that.) The third time because he’d come back from a big meeting where a number of people had interacted with tested positive. I don’t remember about the middle one. He tested positive forever after the first time. I think he finally stopped testing after two weeks even though the test still came up positive.
I was confused by your use of the term “ down” with Covid. I had interpreted as “ down for the count” like in bed, can barely move. Completely asymptomatic Covid is a different animal. I had very very mild symptoms and like your friend tested only because I was around others who tested positive. Who knows how many times many of us would test positive if we tested all the time? Of course that’s true of many diseases. Something many are unaware of. I had studied the history of disease in college and had some friends who didn’t believe me that Polio was asymptomatic in the vast majority of cases until recent news articles discussed that fact.
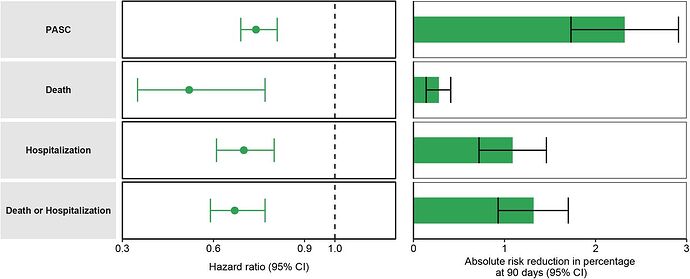
Nirmatrelvir (Paxlovid) and the Risk of Post-Acute Sequelae of COVID-19 (long COVID)
In the VA study, treatment with nirmatrelvir (Paxlovid) was associated with a 26% reduction in risk of long COVID. Risk of death or hospitalization was also reduced.
Risk reduction of specific types of long COVID was also noted.
New preprint estimates that “By November 10, 2022, 94% (95% CrI, 79%–99%) of the US population were estimated to have been infected by SARS-CoV-2 at least once. Combined with vaccination, 97% (95%–99%) were estimated to have some prior immunological exposure to SARS-CoV-2.”
Conclusions and Relevance Effective protection against SARS-CoV-2 infection and severe disease in October 2022 was substantially higher than in December 2021. Despite this high level of protection, a more transmissible or immune evading (sub)variant, changes in behavior, or ongoing waning of immunity could lead to a new SARS-CoV-2 wave.
US had higher COVID-19 and excess all-cause mortality than other rich countries from June 2021 to March 2022.
| If the US’ COVID-19 mortality were like … | this number of US deaths would have been averted |
|---|---|
| New Zealand | 357,899 |
| Canada | 269,401 |
| Finland | 213,546 |
| UK | 174,500 |
| Austria | 154,622 |
| 10 most-vaccinated states | 122,304 |
| 10 least-vaccinated states | -114,138 |
| If the US’ excess all-cause mortality were like … | this number of US deaths would have been averted |
|---|---|
| New Zealand | 465,747 |
| Canada | 358,306 |
| UK | 320,148 |
| 10 most-vaccinated states | 266,700 |
| Austria | 240,871 |
| Finland | 209,924 |
| 10 least-vaccinated states | -158,922 |
I thought this was particularly interesting:
Here are some of the points on which opinions diverge:
-
Cause: Doctors don’t yet know what causes long Covid. They have theories: Perhaps it’s an autoimmune disorder, like lupus or rheumatoid arthritis, whereby the virus is gone but the immune system remains active, attacking healthy cells by mistake; or maybe small blood clots develop in the brain, too small to cause a stroke but big enough to trigger neurologic issues.
-
Key symptoms: Long Covid has been linked to more than 200 symptoms. Shortness of breath, fatigue, and sleep disorders or insomnia are the most common symptoms. Others include anxiety, depression, body aches, headache, heart palpitations and “brain fog” — which describes challenges associated with cognition, like thinking, concentration, communication, comprehension, memory and motor function. Some sufferers [have]organ damage, to the heart, lungs, kidneys, skin and brain.
-
Duration: There’s no consistent definition of how long symptoms must persist for someone to be considered a long Covid patient. For example, the CDC [says] a person has long-haul symptoms if they persist beyond (or start after) one month from an initial Covid-19 infection. The WHO generally [uses] a three-month barometer. Different health clinics may use others still.
What experts do know is that for some, long Covid symptoms can last months or even years. About 15% of people whose ailments persist three months after infection continued to experience symptoms at least 12 months after infection, according to the meta-analysis.
These duration definitions are based on when the symptoms start or persist to.
However, what people concerned about long COVID are probably more concerned about is how long they last (i.e. the end point, not the start point). Long COVID symptoms that go away after a few months are not as concerning as those that last forever, for example. Symptoms that last forever which are disabling or significantly impact quality of life are obviously the most concerning ones.
Yes, totally agree UCBalumnus, that the most important thing for most people would be if these are permanent symptoms. It’s encouraging to see that for 85% of the people who had ailments longer than 3 months, their symptoms cleared up before a year (and hopefully/presumably, for many of those people it was way before the one year cut-off for this analysis). And given that we’ve all seen that many studies and/or clinics consider people who have symptoms lasting as short as 6 weeks after illness to be “long covid”, so they wouldn’t even count in those numbers, it’s pretty clear that this study suggests that well over 90% of long covid sufferers will not have symptoms persisting beyond a year. Obviously up-to-a-year with symptoms is terrible (although of course this includes not just people who have serious debilitating symptoms but also people with barely perceptible symptoms), but overall this strikes me as somewhat comforting compared to some articles I’ve read–clearly the vast majority of people who have long covid do become symptom-free. Sending best wishes for recovery to anyone in the 15%, and hoping that solutions are forthcoming for them.
The CNBC page focused on the economics of long COVID. If 30% get long COVID (out of nearly everyone given the 94% infection rate that has been estimated), and 10% of those have long COVID that lasts more than a year or is permanent, that is still about 3% of the population, which can have a substantial effect on disability (from work) and medical care burden, as well as quality of life.
Yes, although these numbers seem high, it seems like a real stretch to assume that people with long covid are all going to be on disability and/or require medical care and/or suffer any noticeable impact on quality of life. Almost every study I’ve seen on covid that results in these huge numbers (like the 30%) have VERY generous, loose definitions–meaning that if someone feels even a tiny hint of a residual cough, or thinks they have mild headaches slightly more often than usual, or thinks they feel a bit more tired than they did before covid–these are all counted. But none of those people would stop going to work or really seek medical attention. The articles always choose to highlight a couple of anecdotal people who have the most debilitating symptoms–very extreme cases. Wouldn’t it be fun if just once one of the authors of these types of articles chose to highlight someone with long covid who has the slightest of symptoms? That’s just as valid as highlighting someone with extreme symptoms, but of course not as sensational!
I myself am recovering from “long pneumonia” right now (still haven’t had covid yet, knock on wood). I am a bit over 6 weeks out. I was terribly sick for 2 weeks, annoyingly sick for the 3rd week, and since then have had just the slightest whisper of a morning cough and barely perceptible shortness of breath I only notice when exercising. However, if I was to fill in a survey and it asked me if I still have symptoms, I guess I would have to say yes. So I would count as a long-XXXXXX patient (in my case, pneumonia). But I’m not sick and not suffering. I largely feel great and certainly am doing all of my work and activities. I absolutely have no intention of seeing a doctor to talk about these teensy tiny residual symptoms that I’m sure will eventually disappear. This is also true for many of the people who are counted as having long covid. Just because you have long covid does not mean you are completely immobile. Of course, there are those terrible cases of people being disabled, and for long period of times. But that does not appear to be anywhere NEAR 3% of the population!
Although I read the article, I didn’t read the original study that came up with the $3.7 trillion number, but hints in the article make me think it’s likely that the study is based on assumptions that seem overly pessimistic about people who are included in the long covid numbers largely being people who have extreme (debilitating) symptoms. I guess that kind of study generates more attention in the media so may be more rewarding to make those kinds of assumptions.
No one seems to have noticed it, but the Novavax vaccine has been EUAed for booster use in the US.
It is a monovalent vaccine targeted against the ancestral virus. Novavax claims that a BA.1 version and a bivalent BA.1 / ancestral version did not do any better at inducing antibodies to neutralize BA.5 pseudoviruses.
This is more of a medical musing than specifically COVID but there are so many experts I thought I’d throw it out here.
I had picked up a cough earlier in November which ended up as a touch of pneumonia a week ago. I got onto antibiotics right away and have been steadily improving. But normally I’m relatively healthy - an occasional winter cold but never the flu or anything severe.
So I was wondering if pre-pandemic I was routinely exposed to viruses and my body would fight them off without me knowing and I would develop resistance. But since the pandemic, I’ve been fairly careful not to expose myself to anything. Could that actually have left me more susceptible to non-COVID bugs (I am fully vaccinated)?
I think I caught this from my brother or wife who visited us for a couple of days after a trip to Hawaii (and wife’s brother and family). I had understood my brother to be ultra-cautious due to being immunocompromised from CLL. But he had a cough when he was here and both of them subsequently had sinus infections. So maybe he wasn’t as careful as he always claims to be? At least nobody ever tested positive for COVID but seems like we should have been concerned about other stuff.
YLE writes about long COVID effects and risks from various studies: